Your A to Z Guide for Ulcerative Colitis
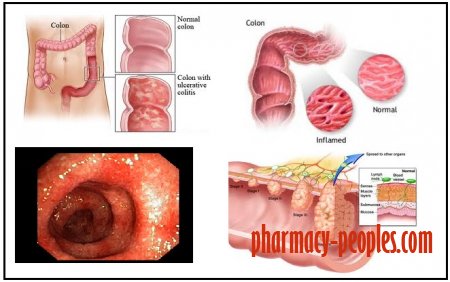
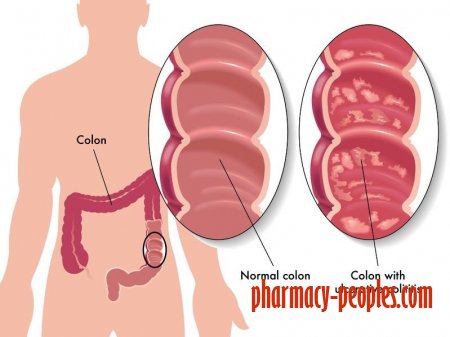
Ulcerative colitis (UC) is a chronic disease in which the lining of the large intestine (colon) becomes inflamed.
The colon then develops ulcers (open sores) that produce blood, pus, and mucus.
The small intestine is rarely affected.
The combination of inflammation and ulcers often causes abdominal discomfort, frequent bowel movements, and bloody stools.
Ulcerative colitis is a type of inflammatory bowel disease (IBD), but it's not the same as irritable bowel syndrome (IBS).
Although the disorders share some of the same symptoms, such as abdominal pain and diarrhea, inflammation or ulcers do not occur with IBS.
Types of Ulcerative Colitis
There are several subtypes of ulcerative colitis, which are named according to the part of the colon affected:
- Ulcerative proctitis, which affects only the rectum
- Proctosigmoiditis, which affects the rectum and lower segment of the colon (sigmoid colon)
- Left-sided colitis, which affects the rectum, sigmoid colon, and descending colon up to the sharp bend near the spleen
- Pan-ulcerative or total colitis, which affects the entire colon
How Common Is Ulcerative Colitis?
Ulcerative colitis affects as many as 900,000 Americans, according to the Crohn's and Colitis Foundation.
Symptoms of the condition most often start between age 15 and 30, with most people diagnosed in their mid-thirties. There’s also a peak between age 50 and 70.
People of European descent have a higher risk of developing ulcerative colitis than those of African or Hispanic descent.
People of European Jewish descent have an especially high risk.
Ulcerative colitis tends to run in families, affecting men and women equally overall. But older men are more likely to develop it than older women.
What Causes Ulcerative Colitis?
Ulcerative colitis is believed to be caused by an abnormal response by your body’s immune system.
Your immune system is supposed to defend you against harmful invasive bacteria and viruses. But in some people, the immune system mistakenly attacks the body’s own tissue.
In ulcerative colitis, this may happen when the body mistakes food and helpful bacteria for harmful substances. It may also come about when the body doesn't turn off its response to fighting an infection.
Either way, the immune system sends white blood cells to the lining of the colon, where they cause inflammation and ulcers.
Experts believe that ulcerative colitis develops due to a combination of environmental factors and genetic predisposition.
While a specific cause is unknown, diet and stress may aggravate the condition.
For example, one study found that a high intake of trans fats — found in many processed foods — raises the risk of ulcerative colitis.
A high intake of omega-3 fatty acids may lower the risk of the condition.
Fatty cold-water fish — such as mackerel, tuna, salmon, sardines, and herring — are rich sources of omega-3 fatty acids.
What Are the Symptoms of Ulcerative Colitis?
The most common symptoms of ulcerative colitis are abdominal pain and diarrhea, which often contains blood or pus.
Symptoms of the disease typically develop gradually and come and go.
Periods without active disease — known as remission — may last for months or even years.
Over time, ulcerative colitis can progress to cover more of the colon. This typically leads to more severe disease and greater symptoms.
To diagnose ulcerative colitis, your doctor will use a combination of your history of symptoms, lab tests, imaging scans, and viewing the inside of your colon using a flexible tube and camera (colonoscopy or sigmoidoscopy).
How Is Ulcerative Colitis Treated?
Medications are the main treatment for ulcerative colitis. Other treatment options include dietary changes and surgery, if necessary.
Drugs for ulcerative colitis work by reducing inflammation in your colon.
You’re likely to need a combination of drugs for optimal treatment. Some drugs are commonly used for maintenance therapy — to help you stay in remission — while others are used to treat disease activity during flares.
Surgery may be necessary if you have disease that isn’t responding well to drugs, or if you have severe complications that require urgent treatment.
It’s most common to remove the entire rectum and colon if ulcerative colitis requires surgery, but more conservative approaches may also be considered.
Drug Treatments for Ulcerative Colitis
There are a few types of drugs used to treat ulcerative colitis.
Aminosalicylates are typically the first kind of drug prescribed for ulcerative colitis. They work by reducing inflammation directly in your digestive tract and can be taken on an ongoing basis.
Corticosteroids — also known just as steroids — are used to treat disease flares. Most drugs of this type work by suppressing the entire immune system, so they can have severe side effects and shouldn’t be taken for long periods.
Immunomodulators limit inflammation at its source in the immune system and are usually used only when aminosalicylates and steroids aren’t enough.
Biologics are the newest type of drug for ulcerative colitis and tend to be used only when other treatments haven’t been effective.
Can Your Diet Affect Ulcerative Colitis?
There’s no known dietary cause of ulcerative colitis, but different foods may aggravate or help limit symptoms of the disease.
You’re more likely to need to change your diet during periods of active disease (flares), when eating soft, bland foods can help limit symptoms like cramping and diarrhea.
During flares, you may also want to avoid or limit high-fiber and high-fat foods, as well as caffeine, alcohol, dairy products, and spicy foods.
If you’re losing nutrients and water in your diet due to diarrhea, you may need to focus on increasing your fluid intake and getting enough calories, protein, vitamins, and minerals from foods or supplements.
Other drugs for ulcerative colitis may include antibiotics and certain pain relievers.
How Is Ulcerative Colitis Different From Crohn’s Disease?
Ulcerative colitis and Crohn’s disease are different types of IBDs that affect the digestive tract in different ways.
There are some common symptoms between the two conditions, but the overall pattern of symptoms tends to be different for each.
While diarrhea and rectal bleeding are more common in ulcerative colitis, Crohn’s disease more often causes severe abdominal pain, nausea, weight loss, and vomiting.
Ulcerative colitis is limited to the lining of the large intestine (colon), whereas Crohn’s disease can affect the entire digestive tract — from your mouth to your anus — and isn’t limited to the inner part of the intestines.
How Ulcerative Colitis Can Affect Your Emotional Health
People with ulcerative colitis are at a higher risk for mental health conditions like anxiety and depression.
While there’s no evidence that stress or tension cause ulcerative colitis, they can affect how you perceive and cope with the disease.
You’re more likely to experience symptoms of a mental health disorder if the ulcerative colitis is more active or severe, as well as during disease flares.
You may also experience flares of your disease more often if you’re anxious or depressed.
If you experience symptoms of anxiety or depression — like bouts of fear or panic, discomfort around other people, or feeling hopeless or uninterested in activities — it’s important to bring them to your doctor’s attention.
Pregnancy Considerations for Ulcerative Colitis
If you’re pregnant or considering becoming pregnant, you may face a dilemma: whether to keep taking your medication for ulcerative colitis.
Some drugs for ulcerative colitis are considered generally safe for pregnancy, although this doesn’t mean they’re totally without risks. Other drugs must be stopped months before you conceive.
But active disease may be the greatest threat to your pregnancy. If you have a flare while you’re pregnant, your baby may not develop properly and may be born prematurely.
And if you end up needing surgery during pregnancy because of active disease, you may risk losing your pregnancy.
Getting Ready for a Colonoscopy When You Have Ulcerative Colitis
Prepping for a colonoscopy can be physically and emotionally draining when you have ulcerative colitis.
The solutions you’re prescribed to drink will make you go to the bathroom a lot and may also leave you feeling exhausted or nauseated.
If you’ve experienced problems with one form of prep in the past, consider asking your doctor about alternative options, since several different laxatives may be used.
Other helpful strategies for getting through your prep may include stopping solid food earlier than directed, giving yourself a fleet enema, drinking your laxative on ice with a straw, drinking lots of water, and going to bed early.
It’s important to develop a treatment strategy for your pregnancy with your doctor, ideally well before you become pregnant.