5 Warning Signs Of Endometrial Cancer Every Woman Should Know
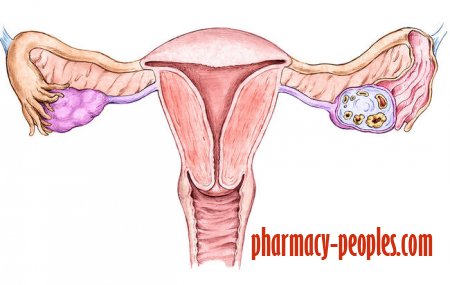
The lining of your uterus, your endometrium, is like a garden bed where a pregnancy can be planted. But other things sometimes grow there, too—including cancerous cells. Endometrial cancer affects more than 635,000 women in the US, but there's no standard screening test designed to catch it.
"Pap tests don't check for or find endometrial cancer, and most women who get it have normal Paps," says Nita Karnik Lee, MD, associate professor of obstetrics and gynecology at the University of Chicago Medicine. In order to detect the disease, your doctor would have to order a transvaginal ultrasound or CT scan (along with a biopsy)—which of course isn't standard or advisable unless there's a strong reason to suspect you might have cancer.
To protect yourself, start by knowing your risk factors: You can get endometrial cancer anytime, but it's most common between ages 45-74. Being overweight, having diabetes, and taking estrogen-only hormones ups your risk. So does going through menopause later than normal or having gotten your first period at an extra young age.
But the most important thing you can do, really, is to know the warning signs. (If you catch endometrial cancer early, it's highly curable.) Here are some worth bringing to your doc's attention:
Vaginal bleeding you can't explain
This is the most common sign that cancer's on board in your uterus, says Lee. In fact, abnormal bleeding happens in 90% of endometrial cancer cases. If you're postmenopausal and all of a sudden you find yourself needing panty protection again, that's not normal. "Women after menopause should not have further bleeding or even spotting," says Lee. Check in with your doctor if you are.
In younger women, heavier than normal periods, periods that last longer than you're used to, or bleeding between periods could be a red flag.
Weird discharge
It's normal to have some discharge from your vagina, but if the amount or color seems different than usual—or if you start spotting between periods and you never used to—it can't hurt to get checked out. If you've recently gone through menopause, you should also know that discharge isn't common after your periods stop for good, so if you're still seeing some let your doctor know.
Pelvic pain that won't go away
Not everyone with endometrial cancer will have pain, but it can show up for some, especially if your cancer has been around for a while. "If the uterus has become enlarged due to the cancer, you may experience pain or cramping," says Lee. Sometimes it can even show up as a mass you can feel in your lower abdomen. You may find it hurts to have sex or go to the bathroom. But the hallmark is constant discomfort, which warrants a visit to your doctor.
Changes in your bathroom habits
Does pressure in your pelvis have you heading for the ladies' room more often? Your bladder and bowels can be a good indicator of uterine problems, and that includes cancer. Cancer might make you need to go more often, have trouble getting urine out, or cause pain when you do go. You might also notice blood in your bowel movements, or it may hurt when you try to pass stool.
Dropping pounds for no reason
If you're experiencing this symptom, it may mean your body's been dealing with a problem for a long time. "Weight loss is rare unless it's more advanced cancer," says Lee. If the numbers are plummeting every time you step on a scale, especially if you have other gynecological symptoms, see your doctor ASAP.
- Health / Disease
- 28-12-2017, 22:09
- 1 531
- Pharmatic