9 Facts Every Woman Should Know About Endometriosis
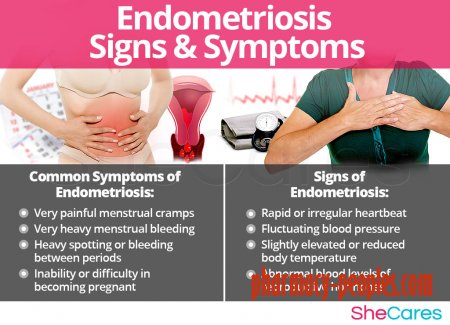
Endometriosis, in which the lining that’s grown inside the uterus each month also mistakenly grows outside the uterus, can cause debilitating pain that affects everything from your work life to your sex life to your fertility. The condition affects about 11 percent of American women, primarily during the childbearing years. Also known as endometrial implants, it can cause pain and inflammation throughout the pelvic area and, rarely, in other parts of the body and result in painful urination or bowel movements, pain during or after sex, long and heavy periods, digestive problems, chronic pain, and fatigue. For some women, endometriosis is also linked with infertility.
Endometriosis, however, is a condition that’s often misunderstood. Here are nine things to know in order to be your own best advocate.
1. There’s actually a lot we don’t know about the condition.
Endometriosis seems to result from some combination of a woman’s own immune system and a genetic predisposition, though experts don’t really know what causes it. Risk factors include starting your period earlier or reaching menopause later, which prolongs your exposure to endogenous estrogen; menstrual cycles shorter than 27 days; never having children, a family history of the condition; or another health problem that affects your menstrual cycle.
2. You don’t need a diagnosis to get treated.
The truth is that treatment is the same for women with endometriosis as it is for women with debilitating menstrual pain who don’t have endometriosis, says Barbara Levy, MD, the vice president of health policy for the American College of Obstetricians and Gynecologists (ACOG), who has had a research interest in pelvic pain and endometriosis for 30 years. “There’s a whole spectrum,” says Dr. Levy, “that goes from discomfort all the way to excruciating and debilitating cramping that’s worse than labor pain that women can experience [whether they have endometriosis or not].”
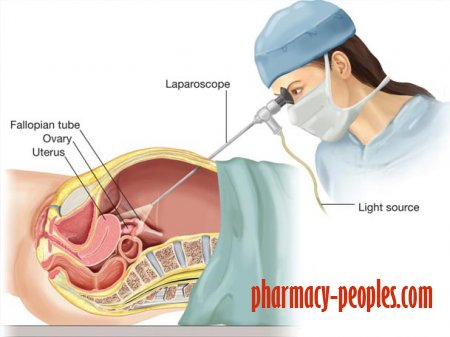
While your doctor should do a thorough pelvic exam and may use ultrasound or MRI imaging to look for endometrial cysts, the only definitive way to diagnose endometriosis is by means of laparoscopic surgery, and possibly a biopsy, in which a small amount of tissue is removed for testing. Even so, “surgery is not a good diagnostic test,” says Sara Till, MD, MPH, a gynecologic surgeon who specializes in chronic pelvic pain and minimally invasive surgery at the University of Michigan in Ann Arbor. “There are risks, it’s expensive, and really bad things can happen — no matter how good your surgeon is.” That’s why most doctors will recommend starting treatment for the pain without a diagnosis, known as empiric treatment. “The decision on surgery should be secondary,” says Dr. Till.
3. Medication can help — but it can take time to find the right one.
Treatment typically includes pain relievers, such as nonsteroidal anti-inflammatory drugs (like ibuprofen) and hormonal medications (like birth control pills), which can slow the growth of endometrial tissue. However, some trial and error may be necessary to find a medication that works for you.
If you don’t find symptom relief within the first month or two of following a given treatment regimen, go back to your doctor and speak up, says Levy. The longer you delay, the higher the risk that the pain will become chronic, she says, and the more challenging it can be to get rid of. Over time, pain can affect the wiring of the brain, she explains, citing — the way some amputees continue to “feel” pain in their amputated limb.
As you work with your doctor, you’ll weigh the risks and benefits of any treatment option before starting a new course of treatment. You may even opt for surgery to confirm your diagnosis before progressing to treatment options that can cause significant side effects. The goal, says Till, is to achieve amenorrhea, or no periods, in order to stem the cycle of bleeding and inflammation.
4. No two women experience endometriosis in the same way.
Just as one woman can go through her period without missing a beat while another may spend a week curled up in the fetal position with a heating pad, some women with endometriosis have no symptoms at all while others experience debilitating pain that affects their life daily. “The vast majority of women find relief,” says Levy. But it’s important for you to find a doctor who listens to you and sticks with you until you find a treatment that works.
5. Your ob-gyn isn’t a one-stop shop.
While academic medical centers are often more attuned to taking a multidisciplinary approach to treating pain, if you live in a more rural area, you may need to take matters into your own hands, says Levy. That means finding a doctor who is able to work with others in the medical community. “Sometimes [that might be] a neurologist who works with migraine people.” Levy says. “Sometimes it’s a rheumatologist who deals with fibromyalgia. And there’s a whole group of specialists who do pelvic floor physical therapy that do a terrific job.”
It’s also not uncommon for women to travel several hours to see a specialist like Till, who treats patients from many nearby states. “I see myself as a consultant who works with your main provider,” she says. “The goal is for patients to graduate from seeing me so they can get care from someone closer to home.
6. Not every symptom you experience should be blamed on endometriosis.
While endometriosis goes hand in hand with many other health problems, it’s hard to determine which symptoms are due to endometriosis, and which might be caused by a condition with the same underlying mechanism. For example, pelvic floor muscle pain, painful bladder syndrome, irritable bowel syndrome — each of these seems to be common among women with endometriosis, but Till stops short of calling them symptoms of endometriosis. “We don’t think endometriosis causes these things, but they do seem to occur in the same people, which makes us think there’s some underlying mechanism that makes these individuals prone to both,” she says. “I address them in tandem. Otherwise, if we blame every symptom on endometriosis, I narrow the treatment plan and miss all the other things that could be going on.”
That may mean that to address your particular symptoms, you should also see a GI specialist, a urologist, or a physical therapist who specializes in the pelvic floor area. “Outside of birth control, of all the treatments I prescribe, pelvic floor physical therapy tends to be the most impactful for my patients,” says Till. The challenge, she says: getting patients to try it. You can find specialists near you at pelvicpain.org.
7. Surgery can help some women — but it isn’t the end of the road.
Surgery can be a tempting fix for endometriosis, and it can help some women with specific symptoms of the condition. But Levy warns that the relief can be temporary, which leads to repeated surgeries — and with each surgery, the pain relief wears off sooner. According to the ACOG, about 40 to 80 percent of women who’ve had surgery have pain return within two years. That’s why the American Society for Reproductive Medicine recommends taking the long road to maximize medical treatment and to avoid repeated surgeries for relief of endometriosis.
As a trained surgeon, Till agrees. “The decision for surgery is not the mainstay of the treatment,” she says. It provides relief for about 70 percent of patients, she estimates, but the problem is how long that relief lasts. “[Surgery is] not going to make pain better on its own.” That’s where working with a physical therapist, GI specialist, or urologist might come in.
8. Endometriosis can affect fertility for some women — but not all.
Approximately half of women with endometriosis struggle to get pregnant. Experts believe that inflammation caused by the condition may interfere with movement of the sperm or movement of eggs through the fallopian tubes, or prevent normal implantation of a fertilized egg. In addition, there’s the fact that the mainstay of treatment is birth control. Luckily, infertility related to endometriosis is highly treatable, or at least can be circumvented with assisted reproductive technologies. What’s more: Because pregnancy is a high-progesterone state, and progesterone can help suppress endometriosis, “many of my patients feel great during pregnancy,” explains Till.
9. You deserve a doctor who listens.
“If you feel as if your doctor is dismissing you, find someone else,” says Levy. “Not all doctors are best suited for managing these complex conditions. But if you’re not feeling listened to and warmly embraced by a physician who wants to help you, you should find someone else.”
- Health / Disease
- 15-03-2018, 22:57
- 1 594
- Pharmatic