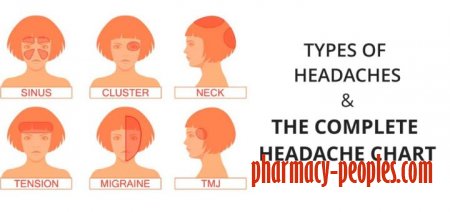
10 Types of Headaches and How to Treat Them
Types of headaches
Many of us are familiar with some form of the throbbing, uncomfortable, and distracting pain of a headache. There are different types of headaches. This article will explain 10 different types of headaches:
- tension headaches
- cluster headaches
- migraines allergy or sinus headaches
- hormone headaches
- caffeine headaches
- exertion headaches
- hypertension headaches
- rebound headaches
- post-traumatic headaches
In some cases, a headache may require immediate medical attention. Seek immediate medical care if you’re experiencing any of the following alongside your headache:
- stiff neck
- rash
- the worst headache you’ve ever had
- vomiting
- confusion
- slurred speech
- any fever of 100.4°F (38°C) or higher
- paralysis in any part of your body or visual loss
If your headache is less severe, read on to learn how to identify the type of headache you may be experiencing and what you can do to ease your symptoms.
The most common primary headaches
These headaches can be episodic or chronic:
- Episodic headaches may occur every so often or even just once in a while. They can last anywhere from half an hour to several hours.
- Chronic headaches are more consistent. They occur most days out of the month and can last for days at a time. In these cases, a pain management plan is necessary.
1. Tension headaches
If you have a tension headache
Anyone can get a tension headache, and they’re often triggered by stress.
An over-the-counter (OTC) pain reliever may be all it takes to relieve your occasional symptoms. This includes:
- aspirin
- ibuprofen (Advil)
- naproxen (Aleve)
- acetaminophen and caffeine, like Excedrin Tension Headache
If OTC medications aren’t providing relief, your doctor may recommend prescription medication. This can include indomethacin, meloxicam (Mobic), and ketorolac.
When a tension headache becomes chronic, a different course of action may be suggested to address the underlying headache trigger.
2. Cluster headaches
Cluster headaches are characterized by severe burning and piercing pain. They occur around or behind one eye or on one side of the face at a time. Sometimes swelling, redness, flushing, and sweating can occur on the side that’s affected by the headache. Nasal congestion and eye tearing also often occur on the same side as the headache.
These headaches occur in a series. Each individual headache can last from 15 minutes to three hours. Most people experience one to four headaches a day, usually around the same time each day, during a cluster. After one headache resolves, another will soon follow.
A series of cluster headaches can be daily for months at a time. In the months between clusters, individuals are symptom-free. Cluster headaches are more common in the spring and fall. They are also three times more common in men.
Doctors aren’t sure what causes cluster headaches, but they do know some effective ways to treat the symptoms. Your doctor may recommend oxygen therapy, sumatriptan (Imitrex) or local anesthetic (lidocaine) to provide pain relief.
After a diagnosis is made, your doctor will work with you to develop a prevention plan. Corticosteroids, melatonin, topiramate (Topamax), and calcium channel blockers may put your cluster headaches into a period of remission.
3. Migraines
Migraine pain is an intense pulsing from deep within your head. This pain can last for days. The headache significantly limits your ability to carry out your daily routine. Migraines are throbbing and usually one-sided. People with migraine headaches are often sensitive to light and sound. Nausea and vomiting also usually occur.
Some migraines are preceded by visual disturbances. About one out of five people will experience these symptoms before the headache starts. Known as an aura, it may cause you to see:
- flashing lights
- shimmering lights
- zigzag lines
- stars
- blind spots
Auras can also include tingling on one side of your face or in one arm and trouble speaking. However, the symptoms of a stroke can also mimic a migraine, so if any of these symptoms are new to you, you should seek immediate medical attention.
Migraines might run in your family, or they can be associated with other nervous system conditions. Women are three times more likely to develop migraines than men. People with post-traumatic stress disorder also have an increased risk for migraines.
Certain environmental factors, such as sleep disruption, dehydration, skipped meals, some foods, hormone fluctuations, and exposure to chemicals are common migraine triggers.
If OTC pain relievers don’t reduce your migraine pain during an attack, your doctor might prescribe triptans. Triptans are drugs that decrease inflammation and change the flow of blood within your brain. They come in the form of nasal sprays, pills, and injections.
Popular options include:
- sumatriptan (Imitrex)
- rizatriptan (Maxalt)
- rizatriptan (Axert)
If you experience headaches that are debilitating more than three days a month, headaches that are somewhat debilitating four days a month, or any headaches at least six days per month, talk to your doctor about taking a daily medication to prevent your headaches.
Research shows that preventative medications are significantly underused. Only 3 to 13 percent of those with migraines take preventative medication, while up to 38 percent actually need it. Preventing migraine greatly improves quality of life and productivity.
Useful preventative medications include:
- propranolol (Inderal)
- metoprolol (Toprol)
- topiramate (Topamax)
- amitriptyline
The most common secondary headaches
Secondary headaches are a symptom of something else that is going on in your body. If the trigger of your secondary headache is ongoing, it can become chronic. Treating the primary cause generally brings headache relief.
4. Allergy or sinus headaches
Headaches sometimes happen as a result of an allergic reaction. The pain from these headaches is often focused in your sinus area and in the front of your head.
Migraine headaches are commonly misdiagnosed as sinus headaches. In fact, up to 90 percent of “sinus headaches” are actually migraines. People who have chronic seasonal allergies or sinusitis are susceptible to these kinds of headaches.
Sinus headaches are treated by thinning out the mucus that builds up and causes sinus pressure. Nasal steroid sprays, OTC decongestants such as phenylephrine (Sudafed PE), or antihistamines such as cetirizine (Zyrtec D Allergy + Congestion) may help with this.
A sinus headache can also be a symptom of a sinus infection. In these cases, your doctor may prescribe antibiotics to clear the infection and relieve your headache and other symptoms.
5. Hormone headaches
Women commonly experience headaches that are linked to hormonal fluctuations. Menstruation, birth control pills, and pregnancy all affect your estrogen levels, which can cause a headache. Those headaches associated specifically with the menstrual cycle are also known as menstrual migraines. These can occur right before, during, or right after menses, as well as during ovulation.
OTC pain relievers like naproxen (Aleve) or prescription medications like frovatripan (Frova) can work to control this pain.
It’s estimated that about 60 percent of women with migraines also experience menstrual migraines, so alternative remedies may have a role in decreasing overall headaches per month. Relaxation techniques, yoga, acupuncture, and eating a modified diet may help prevent migraine headaches.
6. Caffeine headaches
Caffeine affects blood flow to your brain. Having too much can give you a headache, as can quitting caffeine “cold turkey.” People who have frequent migraines are at risk of triggering a headache due to their caffeine use.
When you’re used to exposing your brain to a certain amount of caffeine, a stimulant, each day, you might get a headache if you don’t get your caffeine fix. This may be because caffeine changes your brain chemistry, and withdrawal from it can trigger a headache.
Not everyone who cuts back on caffeine will experience a withdrawal headache. Keeping your caffeine intake at a steady, reasonable level — or quitting it entirely — can prevent these headaches from happening.
7. Exertion headaches
Exertion headaches happen quickly after periods of intense physical activity. Weight lifting, running, and sexual intercourse are all common triggers for an exertion headache. It’s thought that these activities cause increased blood flow to your skull, which can lead to a throbbing headache on both sides of your head.
An exertion headache shouldn’t last too long. This type of headache usually resolves within a few minutes or several hours. Analgesics, such as aspirin and ibuprofen (Advil), should ease your symptoms.
If you develop exertion headaches, make sure to see your doctor. In some cases, they may be a sign of a serious underlying medication condition.
8. Hypertension headaches
High blood pressure can cause you to have a headache, and this kind of headache signals an emergency. This occurs when your blood pressure becomes dangerously high.
A hypertension headache will usually occur on both sides of your head and is typically worse with any activity. It often has a pulsating quality. You may also experience changes in vision, numbness or tingling, nosebleeds, chest pain, or shortness of breath.
If you think you’re experiencing a hypertension headache, you should seek immediate medical attention.
You’re more likely to develop this type of headache if you’re treating high blood pressure.
These types of headaches typically go away soon after the blood pressure is under better control. They shouldn’t reoccur as long as high blood pressure continues to be managed.
9. Rebound headaches
Rebound headaches, also known as medication overuse headaches, can feel like a dull, tension-type headache, or they may feel more intensely painful, like a migraine.
You may be more susceptible to this type of headache if you frequently use OTC pain relievers. Overuse of these medications leads to more headaches, rather than fewer.
Rebound headaches are likelier to occur any time OTC medications like acetaminophen, ibuprofen, aspirin, and naproxen are used more than 15 days out of a month. They’re also more common with medications that contain caffeine.
The only treatment for rebound headaches is to wean yourself off of the medication that you’ve been taking to control pain. Although the pain may worsen at first, it should completely subside within a few days.
A good way to prevent medication overuse headaches is to take a preventative daily medicine that doesn’t cause rebound headaches and prevents the headaches from occurring to begin with.
10. Post-traumatic headaches
Post-traumatic headaches can develop after any type of head injury. These headaches feel like migraines or tension-type headaches, and usually last up to 6 to 12 months after your injury occurs. They can become chronic.
Triptans, sumatriptan (Imitrex), beta-blockers, and amitriptyline are often prescribed to control the pain from these headaches.
When to see your doctor
In most cases, episodic headaches will go away within 48 hours. If you have a headache that lasts more than two days or that increases in intensity, you should see your doctor for assistance.
If you’re getting headaches more than 15 days out of the month over a period of three months, you might have a chronic headache condition. You should see your doctor to find out what’s wrong, even if you’re able to manage the pain with aspirin or ibuprofen.
Headaches can be a symptom of more serious health conditions, and some do require treatment beyond OTC medications and home remedies.